Abstract
Introduction
Lenalidomide maintenance therapy in Multiple Myeloma has been used in order to prolong the Progression-Free Survival (PFS) obtained with any induction therapy through the depletion of residual tumor burden. In this way, it is well established the value of Minimal Residual Disease (MRD) assessed by flow cytometry (FCM) as an independent prognosis factor in Multiple Myeloma. Similarly, patients who become PET-CT negative (when previously they have proved lesions) have better survival outcomes; in fact, this has recently been accepted as a new response criterion.
However, the available data about the complementary use of both techniques in terms of prognosis are limited. The aim of this study is to analyze the prognostic impact of achieving negative residual disease by FCM and PET-CT during Lenalidomide maintenance therapy.
Methods
We retrospectively selected 87 Multiple Myeloma patients from 3 Spanish hospitals (Hospital 12 de Octubre, Hospital Virgen de las Nieves and Hospital Ramón y Cajal). Main selection criterion was to start Lenalidomide maintenance therapy between 2008-2017; the previous induction therapy was heterogeneous. 75% of included patients had previously received an autologous stem cell transplant. We collected data about baseline variables, clinical and biological parameters, therapy administered and FCM and PET-CT assessment at diagnosis, post-induction and during maintenance. Statistical analysis was realized with SPSS 21.0 version (SPSS, Inc., Armonk, NY).
Results
Response at the beginning of maintenance was VGPR or CR in 78% of patients and 48,3% were MRD-. Initial PET-CT was positive in 31%. After a median of 21 Lenalidomide cycles, 32% of patients with initial MRD+ achieve MRD-; meanwhile, 48,1% of patients with initial PET-CT+ become negative.
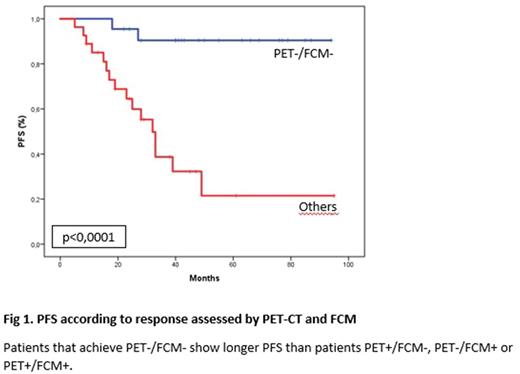
When we jointly assessed FCM and PET-CT results during maintenance therapy (49 patients had been studied by both techniques), we detected a significant difference in terms of PFS between patients that achieve combined PET-/FCM- and the other groups (median PFS not reached vs 32 months, respectively; p<0,0001) (Fig.1). We also found a trend to longer OS in patients PET-/FCM- (4-year OS 100% vs 83%; p=0,053). Patients with standard-risk cytogenetics were more frequently PET-/FCM- than in the high-risk cytogenetics group (31,8% vs 5,6%; p=0,002); nevertheless high-risk cytogenetics patients that achieve PET-/FCM- (n=3) also had prolonged PFS (4-year PFS 100%).
Conclusion
Lenalidomide maintenance therapy increases the proportion of patients that achieve combined PET-/FCM-. Both techniques are complementary and their combination allows us to identify a subset of PET-/FCM- patients with very good prognosis and PFS outcomes significantly superior than the other patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.